Chronic Care Management (CCM) is one of Medicare's most valuable programs for practices managing patients with multiple chronic conditions. Done right, CCM improves outcomes, increases revenue, and strengthens patient relationships. Here's how to build a successful program from the ground up.
Step 1: Identify Your Target Population
CCM requires patients to have two or more chronic conditions expected to last at least 12 months. Run reports from your EHR to identify eligible patients. Common qualifying conditions include hypertension, diabetes, heart failure, COPD, chronic kidney disease, and depression.
Prioritize patients who would benefit most from additional support—those with poor disease control, frequent hospitalizations, or complex medication regimens.
Step 2: Obtain Patient Consent
Before billing for CCM, you must obtain written or recorded verbal consent from each patient. The consent should explain what CCM services include, that only one provider can bill CCM per month, any cost-sharing responsibility, and that they can revoke consent at any time.
Many practices combine consent with enrollment during an office visit or AWV.
Step 3: Design Your Workflow
Effective CCM requires clear workflows. Define who will perform CCM activities (clinical staff, care managers, nurses), how time will be tracked and documented, what activities count toward billable time, when and how you'll communicate with patients, and how you'll coordinate with specialists.
Remember: CCM billing requires at least 20 minutes of non-face-to-face care management time per patient per month.
Step 4: Develop Care Plans
Each CCM patient needs a comprehensive care plan addressing their chronic conditions, medications, and health goals. The care plan should be patient-centered and reviewed/updated regularly.
Good care plans include problem lists and diagnoses, medications with adherence notes, measurable goals, planned interventions, and care team contacts.
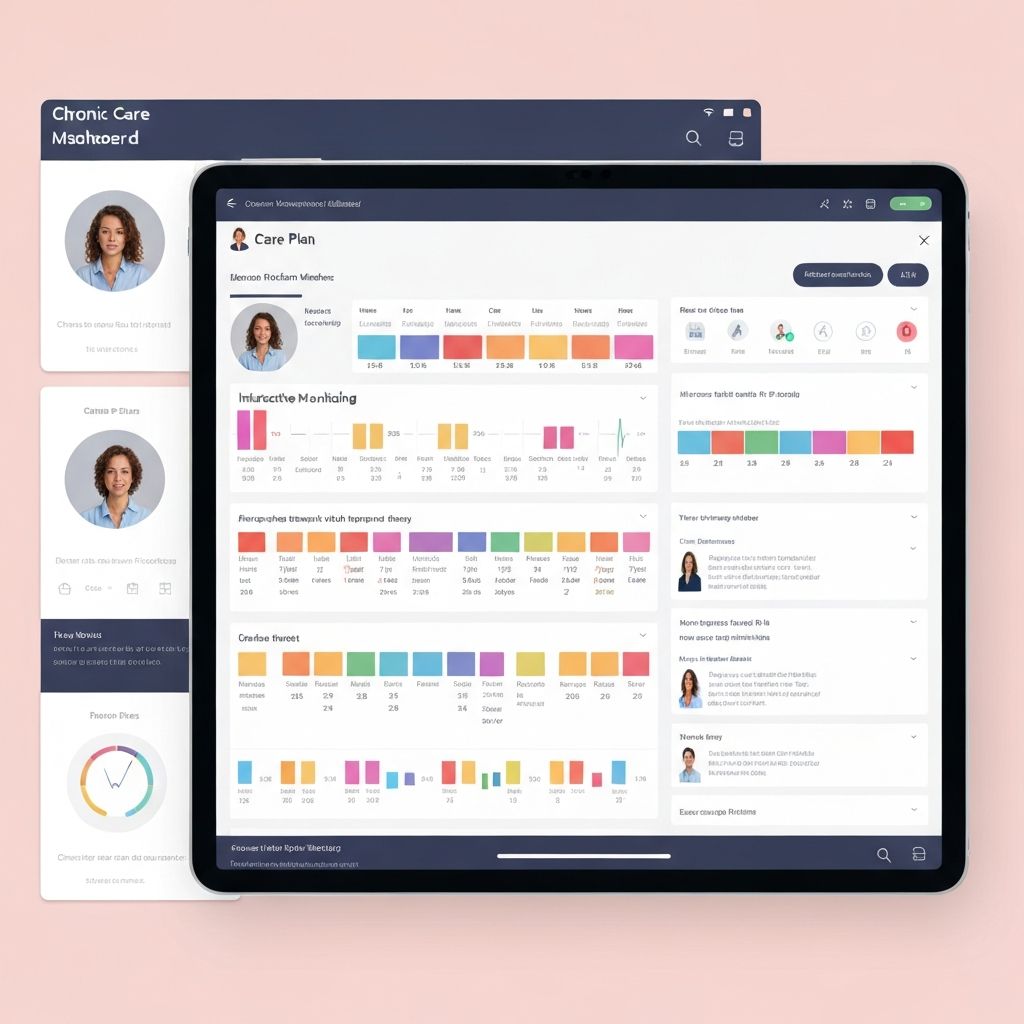
Step 5: Implement Technology
Manual CCM is inefficient and error-prone. Invest in technology that supports patient tracking and outreach, time documentation, care plan management, and communication logging.
A purpose-built CCM platform like Hoss-Kick streamlines these activities and helps ensure billing compliance.
Step 6: Start Small, Then Scale
Don't try to enroll hundreds of patients at once. Start with a pilot group of 20-30 patients. Learn what works, refine your workflows, and then scale systematically.
Step 7: Monitor and Optimize
Track key metrics: enrollment rate, monthly time per patient, billing capture rate, patient satisfaction, and clinical outcomes. Use this data to identify improvement opportunities and demonstrate program value.
The Partnership Option
Building CCM in-house isn't for everyone. Many practices partner with organizations like Hoss-Kick that provide care management staff, technology, and expertise. This approach lets you offer CCM without the operational burden of building and managing a program internally.